Starting a weight loss journey can be both exciting and overwhelming. At Midwest Internal Medicine, we understand that achieving and maintaining a healthy weight is not just about aesthetics—it’s about improving overall health, well-being, and longevity. Our goal is to help you reach your healthiest self through individualized, holistic wellness plans that cater to your unique needs.
Why Striving for a Healthy Weight is Important
Maintaining a healthy weight is critical for overall health and disease prevention. According to the Centers for Disease Control and Prevention (CDC), even a modest weight loss of 5-10% of your total body weight can result in significant health benefits, such as improved blood pressure, cholesterol levels, and blood sugar management .
Here are some compelling facts from well-known health organizations that highlight the importance of maintaining a normal weight:
- World Health Organization (WHO): Overweight and obesity are major risk factors for several chronic diseases, including diabetes, cardiovascular diseases, and cancer .
- American Heart Association (AHA): Individuals who maintain a healthy weight can reduce the risk of heart disease by as much as 50%, lowering their chances of heart attack, stroke, and other cardiovascular conditions .
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Obesity is linked to an increased risk of developing Type 2 diabetes, with research showing that weight loss can prevent or delay the onset of this disease .
- Harvard T.H. Chan School of Public Health: Maintaining a healthy weight is a key component of reducing the risk of certain cancers, including breast, colon, and prostate cancers .
- Mayo Clinic: Weight management through healthy habits like diet, exercise, and stress management is directly associated with improved longevity and quality of life .
These statistics emphasize the importance of achieving a normal weight for health and wellness. But how can you get there? Here are some essential tips that we, at Midwest Internal Medicine, integrate into our patients’ personalized wellness plans.

The Research Behind Our Tips
1. Hydration is Key: Water plays a crucial role in digestion, detoxification, and metabolism. Research shows that drinking adequate water can increase calorie expenditure by up to 30% over a period of 60-90 minutes. Staying hydrated can also reduce hunger and support healthy digestion.
2. Holistic Eating: Eating whole, unprocessed foods helps balance blood sugar levels and provides your body with the nutrients it needs to function optimally. Consuming foods rich in fiber, lean protein, and healthy fats can increase satiety and decrease overeating . In our wellness plans, we recommend limiting gluten and dairy, as they can contribute to inflammation in some individuals.
3. Sleep Matters: Lack of sleep has been linked to increased hunger and weight gain due to the hormone imbalance it causes. A study by the National Sleep Foundation shows that individuals who get less than 7 hours of sleep per night are more likely to struggle with weight control .
4. Managing Stress: Chronic stress leads to elevated cortisol levels, which can increase appetite and cause weight gain, particularly around the abdomen . We encourage patients to incorporate mindfulness practices like yoga, meditation, or grounding exercises into their daily routines.
5. Exercise for Success: Regular physical activity, particularly strength training, is essential for maintaining muscle mass, boosting metabolism, and improving insulin sensitivity. According to the American College of Sports Medicine (ACSM), a combination of aerobic and resistance training is most effective for weight loss .
6. Gut Health: Your gut microbiome plays a critical role in digestion and weight management. Studies show that a healthy gut can improve metabolism and reduce the likelihood of obesity . Probiotic-rich foods like yogurt, kimchi, and sauerkraut can support digestive health and weight loss.
7. Spiritual Wellness: Connecting with your spiritual side, whether through meditation, mindfulness, or spending time in nature, promotes mental and emotional balance. Studies suggest that spiritual wellness can enhance physical health and improve the outcomes of a weight loss journey .
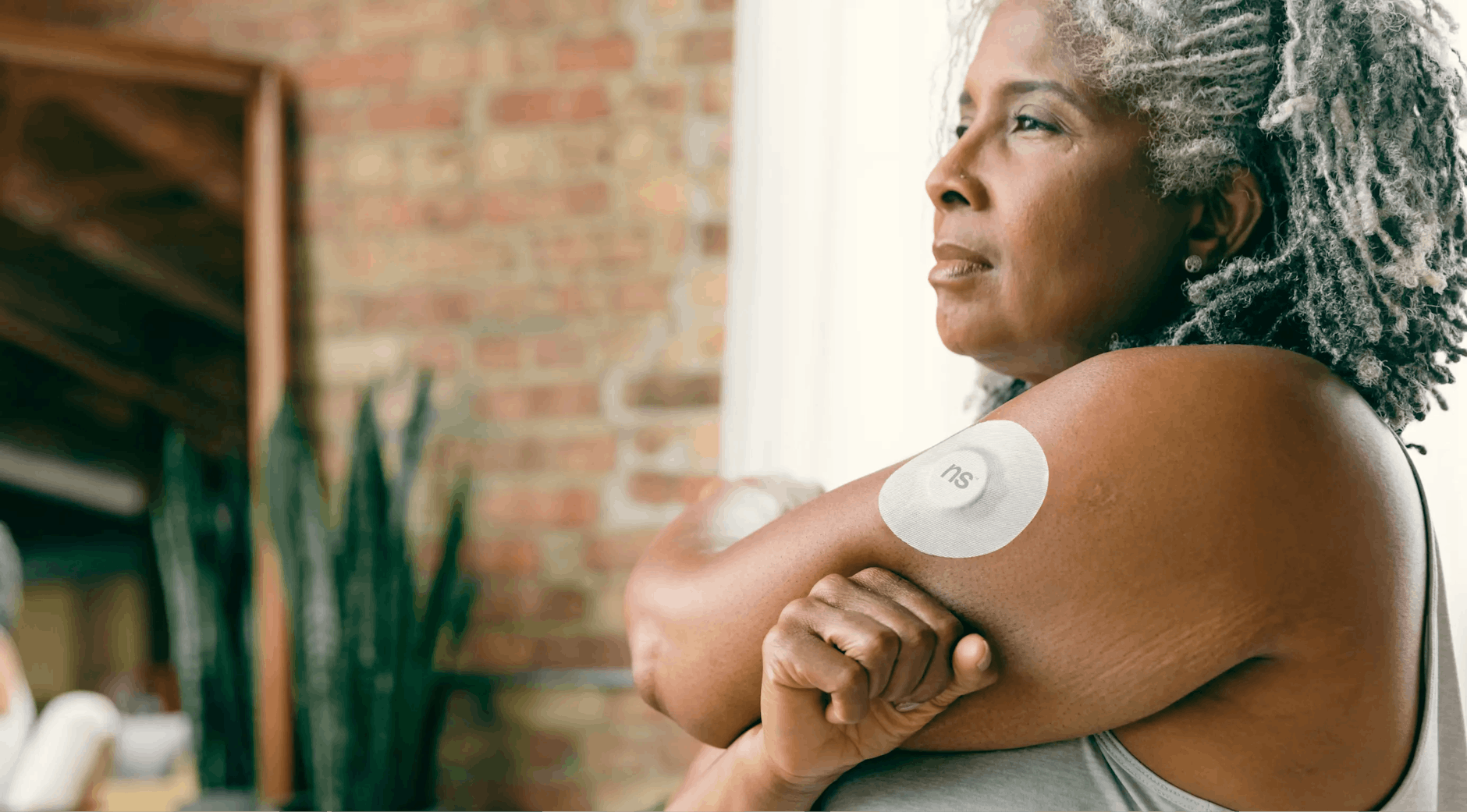
Our Holistic, Individualized Approach at Midwest Internal Medicine
At Midwest Internal Medicine, we believe that every person’s journey to wellness is unique. There is no “one-size-fits-all” solution when it comes to weight loss. That’s why we work closely with each patient to develop a comprehensive, individualized plan that includes nutrition, exercise, stress management, and spiritual wellness.
Our team uses the latest research-backed strategies to help you set realistic goals and maintain healthy habits for life. We’re proud to walk alongside you in this journey and provide ongoing support, adjustments, and encouragement as you work toward your wellness goals.
Just remember!
Achieving a healthy weight is more than just looking good—it’s about reducing the risk of chronic disease, improving your quality of life, and increasing longevity. By following research-backed tips related to hydration, whole foods, exercise, sleep, stress management, and spiritual well-being, you can make sustainable changes that lead to lasting results.

Written By: Roxanne Oliver, DNP, APRN, FNP-BC
*The information contained in this post is for information only. It does not replace routine follow-up and/or care with a certified and licensed medical provider
References
- Centers for Disease Control and Prevention. (2020). The health effects of overweight and obesity. CDC. https://www.cdc.gov/obesity/adult/causes.html
- World Health Organization. (2021). Obesity and overweight. WHO. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- American Heart Association. (2019). Weight management and cardiovascular health. AHA. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022). Weight and diabetes risk. NIDDK. https://www.niddk.nih.gov/health-information/weight-management
- Harvard T.H. Chan School of Public Health. (2021). Weight control and cancer risk. Harvard. https://www.hsph.harvard.edu/nutritionsource/obesity-prevention
- Mayo Clinic. (2023). Healthy weight: Key to longevity. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/weight-loss
- Boschmann, M., & Steiniger, J. (2003). Water-induced thermogenesis. Journal of Clinical Endocrinology & Metabolism, 88(12), 6015-6019.
- Slavin, J. L. (2005). Dietary fiber and body weight. Nutrition, 21(3), 411-418.
- National Sleep Foundation. (2020). How sleep affects weight loss. NSF. https://www.sleepfoundation.org/sleep-and-weight-loss
- Adam, T. C., & Epel, E. S. (2007). Stress, eating and the reward system. Physiology & Behavior, 91(4), 449-458.
- American College of Sports Medicine. (2015). Physical activity for weight loss. ACSM. https://www.acsm.org
- Turnbaugh, P. J., & Gordon, J. I. (2009). The gut microbiome and obesity. Nature, 457(7228), 480-484.
- Koenig, H. G. (2012). Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 2012, 1-33.