Maintaining stable blood glucose levels is one of the most critical factors in achieving not only weight loss but overall optimal health. Blood sugar fluctuations affect your energy levels, hunger cues, mood, and hormones, all of which influence your body’s ability to lose or maintain weight. Let’s dive into the science behind glucose control, its broader impacts on your health, and practical ways to maintain it.
The Impact of Erratic Glucose Spikes on the Body
When you consume foods high in simple carbohydrates or sugar, your blood glucose spikes. This triggers a cascade of hormonal reactions, primarily involving insulin—a hormone produced by the pancreas to help transport glucose into cells. However, erratic glucose spikes can overwhelm the system, leading to several negative effects on the body, especially on the Hypothalamic-Pituitary-Adrenal (HPA) Axis.
HPA Axis Dysregulation and Hormonal Imbalance: The HPA axis is a critical regulator of stress response and hormone production, including cortisol. Studies have shown that frequent glucose spikes and crashes can dysregulate the HPA axis, leading to elevated cortisol levels. This chronic cortisol elevation can contribute to hormonal imbalances such as:
- Increased fat storage, especially around the abdomen.
- Sleep disturbances, as high glucose can interfere with the body’s ability to produce melatonin, the hormone responsible for sleep regulation.
- Gut health issues, as glucose dysregulation can lead to inflammation, impairing gut barrier function and affecting the microbiome.
- Sexual dysfunction, since the endocrine system (responsible for hormone balance) is closely tied to sexual health, including libido and reproductive function.
Long-Term Risks of Uncontrolled Glucose Levels
Over time, poor glucose control can lead to insulin resistance, a condition where your cells no longer respond effectively to insulin, causing blood glucose levels to remain elevated. Insulin resistance has a strong connection to a variety of health issues, including:
- Weight Gain: Persistent insulin resistance often leads to weight gain, particularly around the abdomen.
- Hormonal Imbalance: Insulin resistance disrupts other hormonal systems, including thyroid and reproductive hormones.
- Gut Diseases: High blood sugar levels can foster an environment that promotes gut dysbiosis, which is linked to conditions like Irritable Bowel Syndrome (IBS) and leaky gut.
- Mental Health Problems: Studies have shown a clear connection between erratic glucose levels and mood disorders like anxiety and depression. Glucose spikes lead to inflammation, which has been shown to contribute to these mental health challenges.
Evidence-Based Tips for Balancing Glucose Levels
So how to do you achieve more consistent glucose levels? Every person may be a little different as our bodies are not the same, but some of the tips my patients have found to be helpful include:
- Eat Balanced Meals: Incorporating protein, healthy fats, and fiber with each meal helps slow down glucose absorption, keeping blood sugar levels stable. This has been supported by research from the American Diabetes Association, which emphasizes the importance of balanced macronutrient intake to prevent spikes.
- Choose Low-Glycemic Foods: Opt for whole grains, legumes, vegetables, and other low-glycemic foods, which release glucose more slowly into the bloodstream. According to the Glycemic Index Foundation, low-GI foods can help reduce insulin resistance and support weight loss.
- Exercise Regularly: Physical activity increases your cells’ sensitivity to insulin, allowing them to more effectively use glucose. The World Health Organization (WHO) recommends at least 150 minutes of moderate aerobic activity per week for glucose regulation.
- Stay Hydrated: Dehydration can raise blood sugar levels. Drink plenty of water throughout the day to support healthy glucose levels. This half of your bodyweight in ounces!
- Manage Stress: Chronic stress contributes to HPA axis dysregulation, elevating cortisol and impacting glucose regulation. Meditation, yoga, and deep breathing exercises are all excellent ways to lower stress. I love using the Peloton for this as they have a variety of options to choose from!
Signs and Symptoms of Glucose Dysregulation
So how do you know if you are experiencing high or low glucose levels? Again, this can be different for everyone, but research has shown that there are some common symptoms that people may experience on both spectrums:
High Blood Sugar (Hyperglycemia) Symptoms:
- Fatigue
- Frequent urination
- Increased thirst
- Blurred vision
- Unexplained weight loss
- Difficulty concentrating
Low Blood Sugar (Hypoglycemia) Symptoms:
- Shakiness
- Sweating
- Dizziness
- Hunger
- Irritability
- Palpitations
- Weakness
If you notice these symptoms, it’s essential to seek medical attention and monitor your glucose levels. This is where I like to use a continuous glucose monitor if possible!
Lab Tests to Assess Glucose Control
Let’s talk labs for a second. There a several blood tests that can provide valuable insight into your glucose metabolism, but here are my favorite to trend with my patients:
- Fasting Blood Glucose: This test measures your blood sugar levels after an overnight fast. A normal level is below 100 mg/dL, while 100-125 mg/dL indicates prediabetes, and 126 mg/dL or higher signals diabetes.
- Insulin Levels: Measuring fasting insulin levels can help detect insulin resistance, even if blood sugar levels appear normal. An ideal fasting insulin level is typically below 15 µU/mL.
- Hemoglobin A1C (HgA1c): This test measures your average blood sugar levels over the past 2-3 months. A normal A1c is below 5.7%, prediabetes is 5.7%-6.4%, and diabetes is 6.5% or higher.
*Remember that for fasting levels, these need to be drawn between the hours of 7-9am and on an empty stomach.
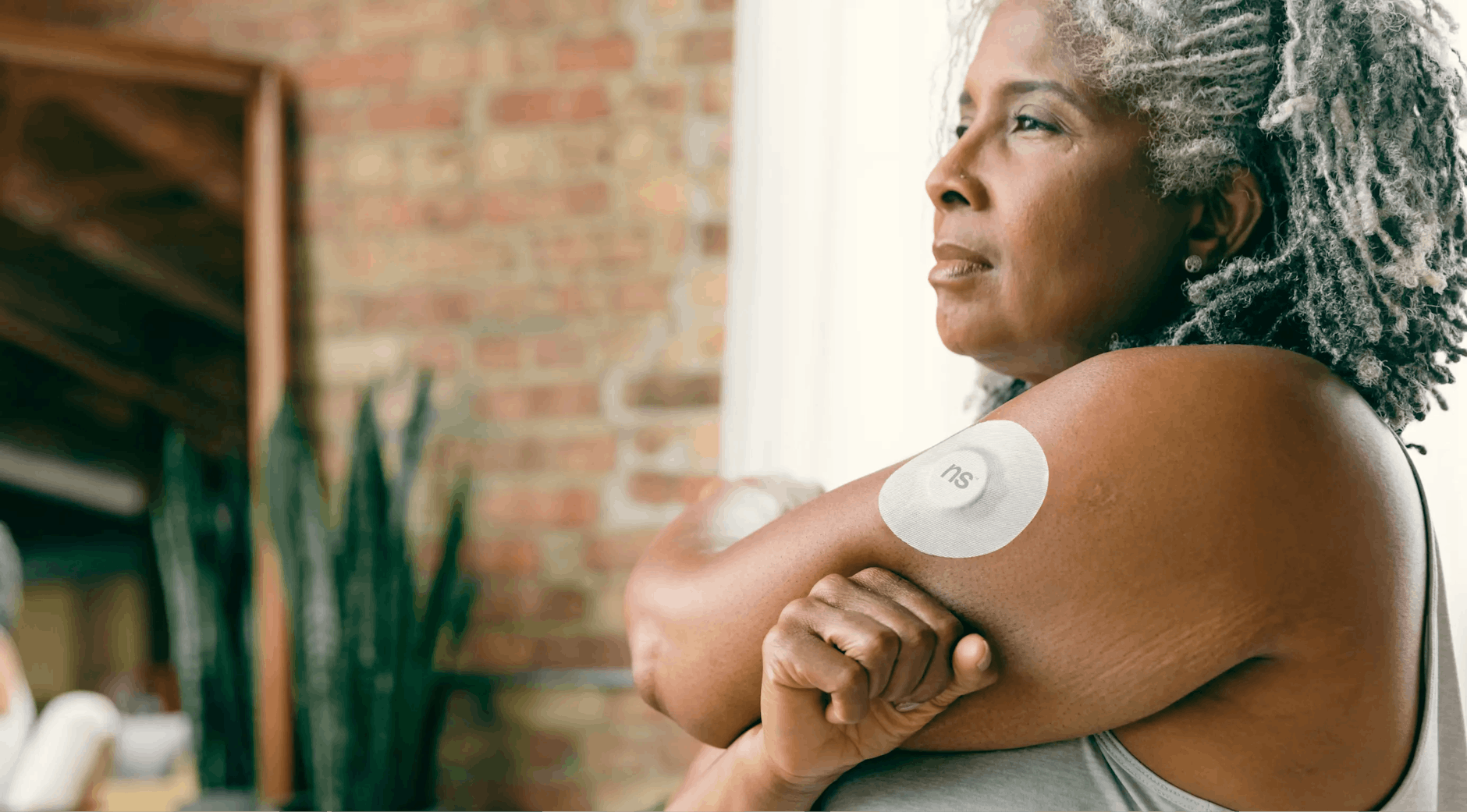
Continuous Glucose Monitors (CGMs): A Valuable Tool for Glucose Control
I have talked a little bit about CGMs before, but let’s do a repeat! For individuals seeking to closely monitor glucose fluctuations, a Continuous Glucose Monitor (CGM) can be an incredibly useful tool. These devices measure glucose levels in real-time and provide a continuous record of how food, exercise, and stress impact your blood sugar (a Dexcom would be an example). Although these are wonderful to use, let’s break down the pros and cons:
Pros of Using a CGM:
- Provides real-time feedback on your diet and lifestyle choices.
- Can identify blood sugar spikes that may not be caught by standard lab work.
- Helps you understand how stress, exercise, and sleep impact your glucose levels.
Cons of Using a CGM:
- They can be expensive and may not be covered by all insurance plans.
- CGMs require frequent calibration and monitoring.
- Some people may experience skin irritation from the device adhesive.
If you are interested in using a CGM I would highly encourage you to speak to your healthcare provider. I do use these periodically in my current practice, however, this is done on an individual basis.
Wrapping it up!
Maintaining stable glucose levels is crucial for weight management, hormone balance, gut health, and overall wellness. Regular monitoring through lab tests like fasting glucose, insulin levels, and HgA1c, combined with tools like CGMs, can offer valuable insights into your body’s glucose regulation. By making small, evidence-based changes in your diet and lifestyle, you can protect yourself from the long-term health risks associated with uncontrolled glucose levels and achieve better overall health.
Take control of your glucose, and in turn, take control of your health!

Written By: Roxanne Oliver, DNP, APRN, FNP-BC
*The information contained in this post is for information only. It does not replace routine follow-up and/or care with a certified and licensed medical provider
REFERENCES
American Diabetes Association. (2022). Standards of medical care in diabetes—2022. Diabetes Care, 45(Supplement_1), S1-S2. https://doi.org/10.2337/dc22-SINT
Cryer, P. E. (2016). The pathophysiology of hypoglycemia in diabetes. Diabetes Care, 39(4), 556-562. https://doi.org/10.2337/dc15-2715
Glycemic Index Foundation. (n.d.). The glycemic index. Glycemic Index Foundation. https://www.gisymbol.com/about-glycemic-index/
International Diabetes Federation. (2021). IDF diabetes atlas (10th ed.). International Diabetes Federation. https://diabetesatlas.org/
Mayo Clinic Staff. (2021). Insulin resistance: What it is and how to know if you have it. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/in-depth/insulin-resistance/art-20047903
National Institute of Diabetes and Digestive and Kidney Diseases. (2020). Hypoglycemia. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/hypoglycemia-low-blood-glucose
Reaven, G. M. (2005). The insulin resistance syndrome: Definition and dietary approaches to treatment. Annual Review of Nutrition, 25, 391-406. https://doi.org/10.1146/annurev.nutr.25.050304.092514
World Health Organization. (2020). Physical activity guidelines for health. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/physical-activity